Resistance Training
As a physio, I often hear these questions:
• “What type of exercise should I be doing to build muscle?
• “I’m going to gym and training hard…but I don’t see the results on the sports field. What am I doing wrong?”
Here’s some food for thought:
In order to obtain maximum muscle growth and see rapid progress it is important to bring 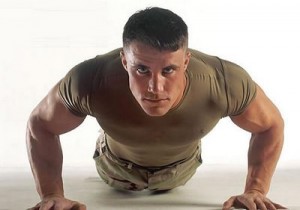 variety into your training and put your body through different kinds of resistance exercises. Body- weight training – working against your own weight – is a great way to train as it does not require any equipment and all of the muscles of the body can be worked. Unfortunately when a lot of people start out, many of them are unable to do pull-ups or push-ups lifting their entire body weight. So it is easier to start
variety into your training and put your body through different kinds of resistance exercises. Body- weight training – working against your own weight – is a great way to train as it does not require any equipment and all of the muscles of the body can be worked. Unfortunately when a lot of people start out, many of them are unable to do pull-ups or push-ups lifting their entire body weight. So it is easier to start  with additional resistance training i.e. using dumbbells or handheld weights. Dumbbells are an extension of body-weight training, but are less restrictive as you can vary the resistance slowly as you get stronger. Stronger athletes can go beyond using only their body weight by increasing the weight of the dumbbells.
with additional resistance training i.e. using dumbbells or handheld weights. Dumbbells are an extension of body-weight training, but are less restrictive as you can vary the resistance slowly as you get stronger. Stronger athletes can go beyond using only their body weight by increasing the weight of the dumbbells.
Elastic Resistance – using the resistance of an elastic band – is also a great way to train as the elastic band provides significant resistance but does not weigh anything (plus they are easy to transport and store at home).
Elastic resistance is very different to the resistance provided by body-weight or dumbbells. The more you pull on an elastic band the greater the resistance, so there will be more resistance at the end (inner range) of the movement.It is very important to maintain control throughout the entire movement – while pulling in and while letting go – and not just let the elastic recoil rapidly back to the starting position at the end of the repetition.
 An important type of resistance – especially for athletes – and one that people don’t focus on much is Plyometric Resistance. Plyometrics bring together the strength gained in the gym and the increase in performance gained by high intensity exercise. It is particularly important for athletes who need muscle reactivity, and can help you transform your strength into explosiveness which is essential on the sports field! Plyometric resistance comes into play when you force your muscles to abruptly stop a movement and then go in the opposite direction e.g. jumping off a box, landing while absorbing the shock, and using it to jump as high and as fast as possible. Very, very important in any plyometric exercise is to limit contact with the floor, movements needs to be fast and explosive!
An important type of resistance – especially for athletes – and one that people don’t focus on much is Plyometric Resistance. Plyometrics bring together the strength gained in the gym and the increase in performance gained by high intensity exercise. It is particularly important for athletes who need muscle reactivity, and can help you transform your strength into explosiveness which is essential on the sports field! Plyometric resistance comes into play when you force your muscles to abruptly stop a movement and then go in the opposite direction e.g. jumping off a box, landing while absorbing the shock, and using it to jump as high and as fast as possible. Very, very important in any plyometric exercise is to limit contact with the floor, movements needs to be fast and explosive!
Too much of a good thing can very easily become a bad thing….same goes for plyometrics. So as soon as you notice that the time of contact with the floor becomes too long and you are slowing down too much, know that you are fatiguing and the set should be interrupted for a slight rest time.
In conclusion, it would not be wise to choose one type of resistance over another but rather to combine all of them into your training routine. The net effect will be putting your body through cumulative resistance training that is superior to a focus only on any one particular method of training.
Happy training 🙂
Andrew@PhysioPRO
BY:
General Health/Fitness
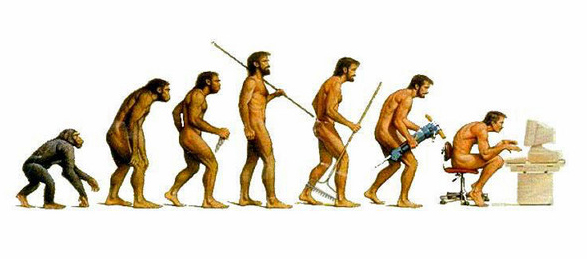
Sitting posture and the (D)evolution of man
FACT: Human beings were not designed to sit for hours on end…
Sitting posture is a constant topic that raises its “crooked” head up at nearly every physio appointment. Why? Well because as physiotherapists, we are constantly battling the negative effects of sitting for hours on end.
The human spine is divided into 4 distinct curves: neck (cervical), middle (thoracic), lower back (lumbar) and sacrum. These curves are designed to distribute the load that gravity places on the spine (like a spring), absorb shock and obviously allow movement.
The problem with sitting is that these curves are “imbalanced”. The neck and middle back curves become exaggerated and the lower back’s curve is almost completely lost (see pic above). This results in adaptive muscle shortening or stretching, depending on which side of the curve we look at. This then translates to poor standing posture and difficulty with functional movements, with the end result being an injury. So what im trying to say is the way you sit at your desk could very well be the reason why you pulled your hamstrings whilst you were running….
Another scary fact is the amount of pressure that you place on the discs (the “cushions” between the vertebras). As you can tell from the diagram above, the difference in pressure between standing and forward lean sitting (i.e. sitting on the edge of your chair leaning forwards) is an ASTONISHING 90% increase!!!! That’s the equivalent of having someone with your own body weight standing on your head!!!
So what can you do if you are one of those office bound monkeys? Well, start off by assessing your posture by comparing it to the “ideal” posture below. Make changes where you can and stick to those. You can have the most expensive “ergonomically” designed office chair, but if you’re not sitting in it properly it’s worthless.
Secondly, STAND!!! Every 30-40minutes, get up and walk around, or if you have some privacy try stretching a bit. Try standing whilst you talk on the phone or walk over to that colleague to deliver a message rather than sending an email.
Look out for my next article on some of the stretches you should be doing at the office or home to improve your posture.
Regards
Ric@PhysioPRO
BY: Riccardo Vaccaro
Back injuries / General Health/Fitness / Neck injuries

First Aid CPR “HARD and FAST”
While not typically physiotherapy-related I thought it important to write on something everybody should know a little bit about – First Aid.
First Aid refers to emergency assistance given to an injured or ill person using readily available materials. This aid ranges from something as basic as removing a splinter from a child’s finger and putting on a plaster on the wound to giving care to casualties of a motor vehicle accident and handing them over to a medical team.
As you can imagine this is a broad area to cover. This article will touch on the basics of First Aid administered on an unconscious adult patient. Overall, I strongly recommend attending a First Aid course as you never know when this key knowledge could help to save a life!
First Aid always aims to:
- Preserve life
- Prevent the illness or injury from becoming worse
- Promote recovery
If in a situation where a patient is unconscious the first thing to do is quickly assess the area for any hazards. You will be no help to the person if you rush into a potentially risky scenario and injure yourself in the process adding to the casualty count. Once the area is safe ascertain the patient’s unresponsiveness by talking to them – (ask and say ‘Hello?’) and then ask for assistance (call loudly for ‘Help’) to get someone to contact the emergency services. The sooner you get the patient medical attention the better! When deciding between calling an ambulance and transporting the patient yourself to the hospital, remember to ALWAYS preferably call an ambulance if you can. An ambulance is well equipped and the patient benefits from immediate medical help when trained paramedics arrive.
Administering CPR (Cardio-Pulmonary resuscitation):
While waiting for the ambulance, if an adult has collapsed and is unresponsive take 5 to 10 seconds to feel for a pulse. This is done by placing two fingers on the patient’s carotid pulse where we feel for the artery found just below the angle of the jaw.
If no pulse is felt ask a fellow bystander to contact the emergency services while you begin CPR as follows:
- Begin with chest compressions over the middle to lower half of the sternum (breast-bone).
- Interlock your fingers and keep your elbows locked straight.
- Press HARD and FAST.
- You must press the chest down at least 5cm with each compression.
- Remember to allow the chest to recoil between compressions.
- Compress at a rate of at least 100 compressions per minute (believe it or not, this rhythm corresponds nicely with the beat of the Beegees’ hit “ Staying Alive”… I can hear you tapping your feet!)
- If you have a barrier device available (mask or one-way protective valve to protect you from blood and air-borne pathogens) you can interrupt compressions to give 2 breaths after every 30 compressions. When giving breaths ensure that you see the chest rise with each breath you give. If no barrier device is available it is acceptable to provide “hands-only” CPR – unless you are comfortable providing mouth to mouth breathing to the victim.
Automated Electronic Defibrillators
Many public places such as gyms and airports have access to Automated Electrical Defibrillators (AED’s). Always call for one of these to be brought to a victim of cardiac arrest as soon as possible. Do not be frightened of using such a device as it is voice prompted and very user friendly. Once an AED has arrived turn it on and attach the pads to the victim by following the voice prompts. Always minimize interruptions to your chest compressions even when applying the AED. Follow the instructions of the AED.
The AED will analyze the patient’s heart and will do one of two things:
1: Recommend a shock – if a shock is required the AED will advise to keep clear of the patient and direct you to press a button to give the patient a shock. After the shock has been administered you must immediately continue CPR, starting with chest compressions.
2: No shock advised – If the AED does not recommend administration of a shock immediately continue with chest compressions until the AED commands “Re-analyze”
When contacting emergency services for a patient undergoing CPR make sure to be as specific as possible about the scenario and let the emergency services know that CPR is underway. This will help prioritise your call at the dispatch office/call centre.
Key points:
Early activation of emergency services, good quality CPR (push HARD, push FAST) and early access to an AED.
If the victim resumes breathing and has a pulse place them on their side in what is called ‘the recovery position’. If they don’t resume breathing continue CPR until medical help arrives.
Useful First Aid courses are regularly held by the St John’s Ambulance Service and the academy of advanced life support {www.stjohn.org.za}
Emergency Services contact numbers: Netcare911 (082-911), ER24(084-124), Gauteng EMS (10177) or dial 112 or 911 from any cellphone.
CPR saves lives.
If you don’t believe me ask Vinny Jones. Watch www.youtube.com/watch?v=JR0aZX1_TD8 and remember ‘push hard and fast to ‘Staying Alive’!’
BY:
General Health/Fitness

Tip of the WEEK
I thought I would just share a neat little trick that I teach most of my patients to manage their own muscular issues. Its so easy and effective that most of my patients end up saying ,”Why didn’t I think of that??”.
All you need is a wall or floor and a tennis ball….Place the tennis ball against the wall or floor (depending on the area you are treating) and then find that knot (trigger point) with the ball. Now apply pressure to the area using your body weight.
You want to apply a even steady pressure at first, till you feel a moderate ache and hold it there. You should feel it easing off after 30-45 seconds, so either push harder or find a new spot. If you feel up to it, you could even rub up-and-down or side-to-side over the ball to free up that tissue.
Whats so great about this technique is that YOU can decide how much pressure to apply and the ball never gets tired (unlike your partner). This also works great for loosening up stiff muscles after a heavy training session. Just make sure you are not doing this with an acute muscle tear (i.e. a “pulled” hamstring) as it could cause further damage.
So there you have it, your very own “physio” that fits in the palm of your hand and you can even take him on holiday with you…
Ric@PhysioPRO
BY: Riccardo Vaccaro
Back injuries / General Health/Fitness / Lower Limb injuries / Upper Limb injuries

Total Hip Replacements
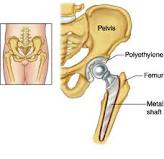
A Total Hip Replacement – or THR as we like to call it in this business – is a surgical procedure in which diseased cartilage and bone, located at the head of the femur and acetabular cap, are replaced with artificial materials (a prosthesis).
More often than not, this is an elective procedure. Therefore, many older patients come to me for advice on whether or not to go for a THR. What I always tell them is that as with any surgical procedure there are potential risks, so it should not be entered into lightly and should be seen as a last resort. In my opinion, the biggest factor is how the operation will affect quality of life. If one’s current hip condition is impairing function to a significant extent – such that quality of life is severely diminished – then a THR would be of great benefit.
Who needs a THR?
- Patients with severe Osteoarthritis
- Patients who have tumours in the hip that have destroyed the hip joint rendering it dysfunctional
- In cases of avascular necrosis (hip joint is destroyed due to lack of blood supply) can develop due to fractures, drug and alcohol abuse and other diseases.
- Patients with intense chronic pain persists despite the use of anti-inflammatories for more than 6 months, adversely affecting sleep, ability to work and movement.
A THR is not recommended for patients with:
- A current hip infection
- Paralysis of quadriceps
- Severe blood disease
- Nerve disease affecting the hip
- Severe mental dysfunction
- Morbid obesity i.e. weighing more than 140kg
If possible, once one has decided to have the operation, it would be of great benefit to start pre-operative strengthening exercises to assist with rehabilitation post-surgery.
To prevent post operative risks, rehabilitation starts immediately after the operation. This includes circulatory and isometric exercises. On Day 1 post-surgery patients are usually sitting up, out of bed and working on strengthening the quadriceps. By Day 2 patients are walking with an assistive device (normally a walker). Physiotherapy is critical in the coming months to regain strength and functional activity.
For the first 3 months post-surgery it’s prohibited to lie on one’s side or cross one’s legs as the hip could dislocate in these positions. After 6 months normal daily activities should continue comfortably.
Always remember to inform your health care professionals that you have had a THR and avoid strenuous activities, running, contact sports etc as this will decrease the life span of your THR. Swimming is a very good way to strengthen and increase the mobility of your hip without causing too much strain on and friction at the joint.
Andrew Savvides
PhysioPRO
BY:
General Health/Fitness / Hip injuries / Lower Limb injuries

Don’t just POP that PILL!
Having repeated this bit of info over and over again to a lot of my patients, I decided its time to put it in writing….
Lets me just start off by saying, Anti-Inflammatories are over-prescribed! At the first sign of any pain or swelling, a doctor will usually pull out his/her referral pad and write a script for anti-inflammatories without giving it a second thought. DON’T POP THOSE PILLS!
Worldwide, 73 000 000 prescriptions of Nonsteroidal anti-inflammatory drugs (NSAIDs) are written yearly. Although theses drugs are very useful at relieving pain, decreasing inflammation, decreasing elevated body temperature, and decreasing blood clotting they are also associated with frequent and significant side effects.
The two main problems with the prescribing of NSAIDs are (1) the TIMING of use and (2) the RELEVANCE to the tissue/injury being treated.
(1) Taking NSAIDs during the acute stage of an injury (usually 48-72hrs) is usually not recommended as this STOPS the inflammatory process. Inflammation is the first key step to tissue healing, so by STOPPING this phase, you are delaying the tissue healing process. Rather LIMIT this phase using the PRICE principles (see our previous article “Acute Injury Management”). Taking NSAIDs in the later (regenerative) phase of healing has also been shown to impede regeneration and increase fibrosis in tissue.
That said there is a narrow window period (the sub-acute phase) where NSAIDs could be used. This is usually 72hrs-10days post injury, but could vary depending on the injury and person.
(2) Understanding the injury/pathology- Of considerable importance to us in the Sports Medicine field are the side effects related to impaired healing in ligaments and bones. Ligament injuries treated with NSAIDs in the acute phase have been shown to have up to a 32% decrease in tensile strength, and fractures have been shown to be 5 times more likely not to unite following NSAID use!! But your doctor gave you NSAIDs for that ankle sprain right???
Tendinopathies (like Achilles tendinopathy, Tennis Elbow etc.) are not inflammatory conditions, so the prescribing of NSAIDs in these cases are useless and can only have negative side-effects. Acute muscle tears are another instance where one should rather avoid NSAID’s as they have been shown to delay healing. However, chronic inflammatory conditions like Rheumatoid Arthritis and Tenosynovitis (inflammation of the tendon sheath) do benefit from NSAID use.
So what’s the take home message?
NSAIDs are effective, but their application to specific tissues and injuries are complex, so don’t rush off to the pharmacy and buy them without first consulting your Sports Physio or Physician.
If you do have a musculoskeletal injury, first take Paracetomol (as found in Panado), as it is effective in relieving pain but without the side effects on tissue healing.
If you are not sure, avoid NSAIDs for the first 3 days post injury and don’t take them for more than 7 days without consulting a health professional.
Ric@PhysioPRO
BY: Riccardo Vaccaro
General Health/Fitness

The trouble with being immobile
Our bodies were designed to move and participate in the different activities of daily living. So what happens when we, recovering from an injury or illness, find ourselves restricted to bed rest for a prolonged period of time? The way in which immobility affects our body and what we can do to prevent the associated complications, is worth exploring further.
Effect on the Cardiovascular system (heart and blood vessels)
Any activity of the muscles will push blood through your body. This blood flow through your veins and back to your heart will increase your circulation. So, when you are just lying in bed and not using those muscles, one risks peripheral oedema – swelling of your hands and feet.
Furthermore, being immobile for prolonged periods will see your resting heart rate increase as the heart needs to work harder to pump the blood through your body, without help from the body’s natural movement and muscle contractions. There will also be a decrease in the ability of the blood to take up oxygen, which can cause you to become dizzy or faint especially when u stand up after prolonged bed rest (postural hypotension).
Deep Vein Thrombosis is a serious complication associated with immobilisation. Which occurs due to an increase in the viscosity(thickening) and slowing down of the blood which basically forms a clot in the vessel. Dislodgement of a venous clot that lodges itself in the lung tissue is called a Pulmonary Embolism and may be fatal.
Effect on the Respiratory System
We all have fine little hairs in the airways that sweep secretions like mucous, phlegm etc upward and out of our respiratory systems. But immobilisation reduces the action of these cilia, or little hairs, and this inability to clear secretions may lead to infections such as pneumonia
Lung collapse (Atelectasis) – especially in the basal lobes of the lung – can also result as respiratory secretions accumulate in these lower lobes in the gravity dependent position and cause the small airways to close.
Effect on the Metabolic system
Prolonged bed rest causes the bones to lose calcium and potassium, as oesteoblastic activity(bone development) is reduced due to the lack of weight going throught the bones. This causes a decrease in the bone integrity or density of the bone matrix perhaps resulting in osteoporosis.
One may also develop kidney stones due to pooling of urine in the kidneys and bladder.
Effect on the Musculoskeletal system
It’s pretty obvious that if you not using your muscles that they will atrophy and weaken. Joint contractures – restrictions in the normal range of motion caused by peri-articular and intra-articular connective tissue – can occur. Basically your joints get stuck!
Another major complication of immobility is the possible development of pressure sores. These develop due to unrelieved pressure especially over areas where the skin lies close to bone. Pressure sores cause tissue death (necrosis). Once developed, these sores take a long time to heal and can be a source of secondary infection in the body.
Effect on the mind
To add to all these negative physical as well as physiological complications, being immobile affects one emotionally. People may have increased anxiety and depression and a decreased attention span.
What can you do?
Nearly all of these complications can be prevented with the right exercises and with help from your physiotherapist.
Undertake active circulatory exercises often, during the day, including foot pumping, static quadriceps and gluteal contractions, and active hip and knee exercises. These will all help to increase your circulation and benefit your cardiovascular system.
To deal with any respiratory problems work on increasing the efficiency of the lungs through deep breathing exercises and physiotherapy to the chest.
Weight bearing exercises are essential to prevent weakening of bones. Start getting out of bed and being mobile as soon as possible. While immobile, undertake exercise programmes that offer resistance training, either with your physiotherapist or using free weights.
As much active movement as possible should be facilitated, to make sure your muscles don’t weaken and shorten, always ensuring that the exercise is carried out to include its full range of motion to prevent contractures.
Ensure pressure relief, particularly on areas where the skin lies close to bone, by changing position every 2 hours, to prevent pressure sores and secondary infection.
It is also very important to try stay positive and motivated in this time of immobility. Speak to people, family, friends even your health care professionals. Set goals for yourself and your recovery and achieve them.
Until next time…Stay ACTIVE!
Andrew Savvides
PhysioPRO
BY:
General Health/Fitness
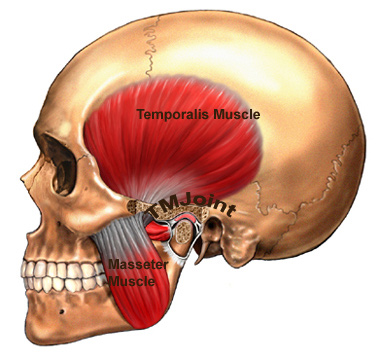
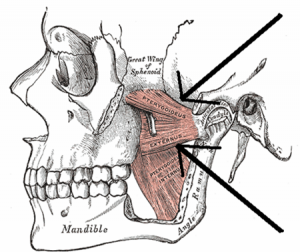
The TMJ- the little joint with a large role
The Temporomandibular joint (TMJ) is a little joint with a big name and even larger role to play in day to day life. It’s found between the jaw bone and one of the bones in the skull – just below the temples.
When one considers how much we use this joint in daily activities it isn’t very surprising that this joint is subject to wear and tear. This, because it’s involved in chewing and talking (ceaseless activities for some). The TMJ can even be damaged while a person sleeps, as clenching or grinding one’s teeth will cause the joint’s cartilage lining to wear away.
Common causes of TMJ dysfunction are:
- Poor posture i.e. one that sees the chin poke out
- Habitual or excessive chewing of gum
- Previous trauma to the area
- Dental problems
- Stress and clenching of teeth
TMJ dysfunction could see people experience limited motion and a general dull ache over the side of the face as well as local muscle tenderness. A ‘click’ may also be present as patients open and close their mouth, as the joint dislocates and relocates back into place. Headaches, sinus and neck problems can all be associated with TMJ dysfunction. It’s clearly a very important joint to keep clear of damage.
A quick self test for TMJ health:
- Place 3 fingers vertically into your mouth. Inability to do this indicates TMJ hypomobility.
Using physiotherapy to treat damage to the TMJ involves:
- myofascial release
- massage
- gentle stretches
- accessory mobilizations
- electrotherapy
- postural correction
- re-education.
Most important is identifying and addressing the cause of the dysfunction.
So if you think you are having problems in this particular area, do not fear. Help is always at hand. Visit your PhysioPRO practice for an assessment.
Until next time…Keep Smiling 🙂 and chewing and talking.
Andrew Savvides
PhysioPRO
BY:
General Health/Fitness / Neck injuries

Effective ways to limit the risk of sports injuries
As all sports persons can attest, injury (or the risk thereof), and fear are the biggest concerns that may severely hinder performance and progression within sport. All sport carries an innate risk of injury, but it is very important for the sports enthusiast to bear the following in mind to limit the risk of injury moving into the new season…
It is essential to know where you are, to get where you want…
Do not overdo it from the get-go.
It is essential to know your current fitness level (which can be assessed by a physiotherapist), in order to plan and execute an appropriately graded training regimen moving into the season. The amount of training can play a key role in determining your injury risk. Fatigued muscles do a poor job of protecting their associated connective tissues, increasing the risk of damage to bone, cartilage, tendons and ligaments. In essence, when starting a new training programme, the loads of enthusiasm could lead to doing too much, too soon, increasing the risk of injury.
Warm Up Before Exercise
Many people are injured in the first few minutes in the gym, on the field or road etc, because they start too hard, without a proper warm-up. Always take 10-20 minutes to warm up gradually before going hard, especially before interval training or any high intensity form of training. A simple warm up can consist of brisk walking, jogging or simply doing your sport at a very slow pace to start.
Correct Diet for Exercise
Eating correctly is essential for energy to workout, a meal about 2 hours before exercise helps you get the most out of training sessions. Eating appropriately after exercise allows for tissue nutrition and optimal recovery for the next workout.
Drink enough water to stay well hydrated
Just a bit of dehydration will decrease your exercise performance which could then also lead to injury. Drink water according to the length and intensity of your exercise sessions. It’s recommended that you drink about 500-750ml water within two hours of exercise, and then drink a cup every fifteen minutes during exercise. If you exercise more than 90 minutes, you will need to add some simple carbohydrates (food or sports drinks) to replenish glycogen (stored glucose energy) stores.
Don’t Exercise with Pain
Exercise shouldn’t cause pain, stop exercising as soon as you experience acute or sharp pains. Pain is usually the body’s way of alerting us of some problem within the body. Pushing through this initial sharp pain may be a fast way to develop a severe or chronic injury. If you don’t feel well, it is a sign that you need some time off until your body heals.
With the repetitive pounding the body and its various systems take with training it is essential to allow time for rest. Rest is an essential component of the repair and regenerative process that leads to healing, growth and strengthening of new and previously damaged tissues.
Mix it up
Another way to prevent injuries is by cross training. Doing the same routine continuously lends the risk for overuse injuries, not to mention boredom and loss of focus. Training various muscle groupings also limits the risk of biomechanical injuries often caused by muscle imbalances. Cross train with other sports, yoga/stretching or resistance training as you can get a full body workout without over-stressing specific muscle groups.
Wear the Right Safety Gear for your Sport
It goes without saying that protective gear such as Helmets, protective pads, mouth guards, sun-glasses, and other specified gear designed to protect against common sports injuries are essential. Athletes should take advantage of this simple way to prevent the most common injuries. Never play without your recommended safety gear.
BY:
General Health/Fitness